



WHAT IS PSORIASIS
- It is a genetic autoimmune disorder
- Transmitted from parents to offspring
- The immune system and genetics play major roles
- Is not contagious. Nor is it caused by infectious bacteria. It cannot be spread from one person to another by touch or other close contacts.
- There is no cure for psoriasis but can be controlled with medications, diet and healthy lifestyle
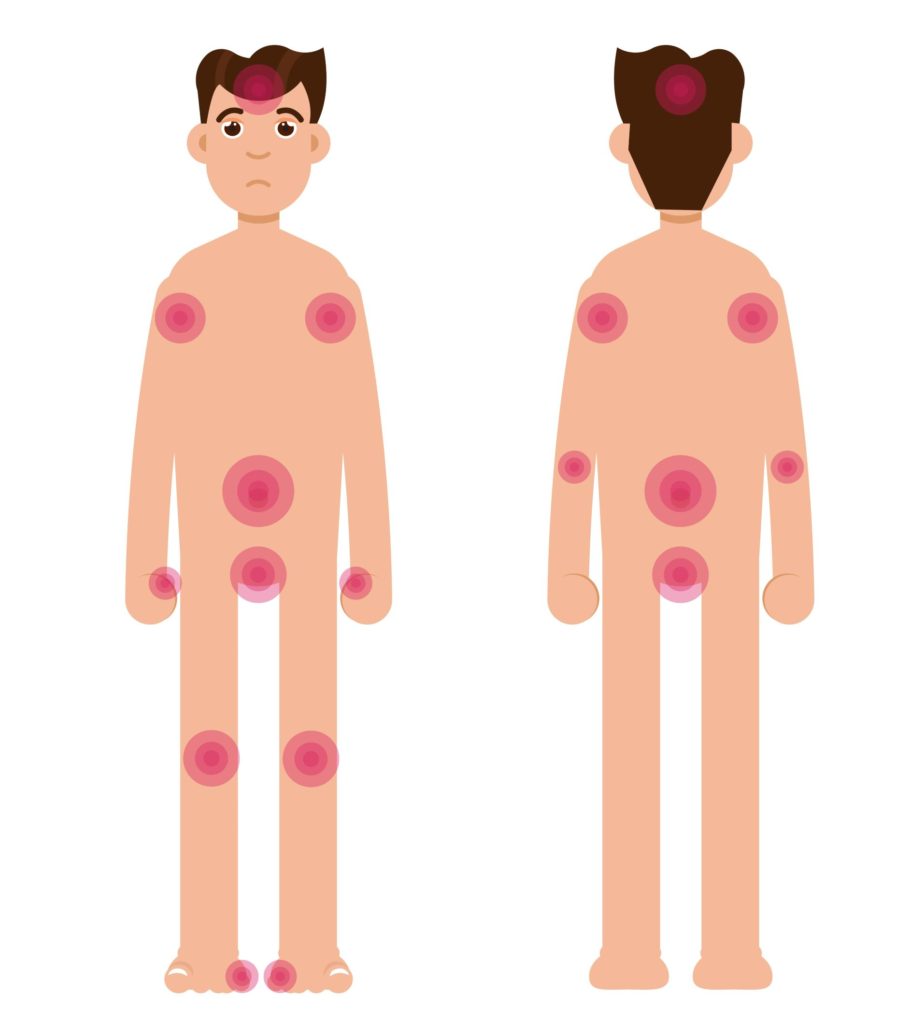
- The affected skin area is normally red, inflamed, scaly, and very itchy. They pop up as patches, plaques, blisters or rash.
- They usually appear on your hands, feet, elbows, knees, scalp, knuckles, scalp, lower back, and skin folds but they can show up anywhere.
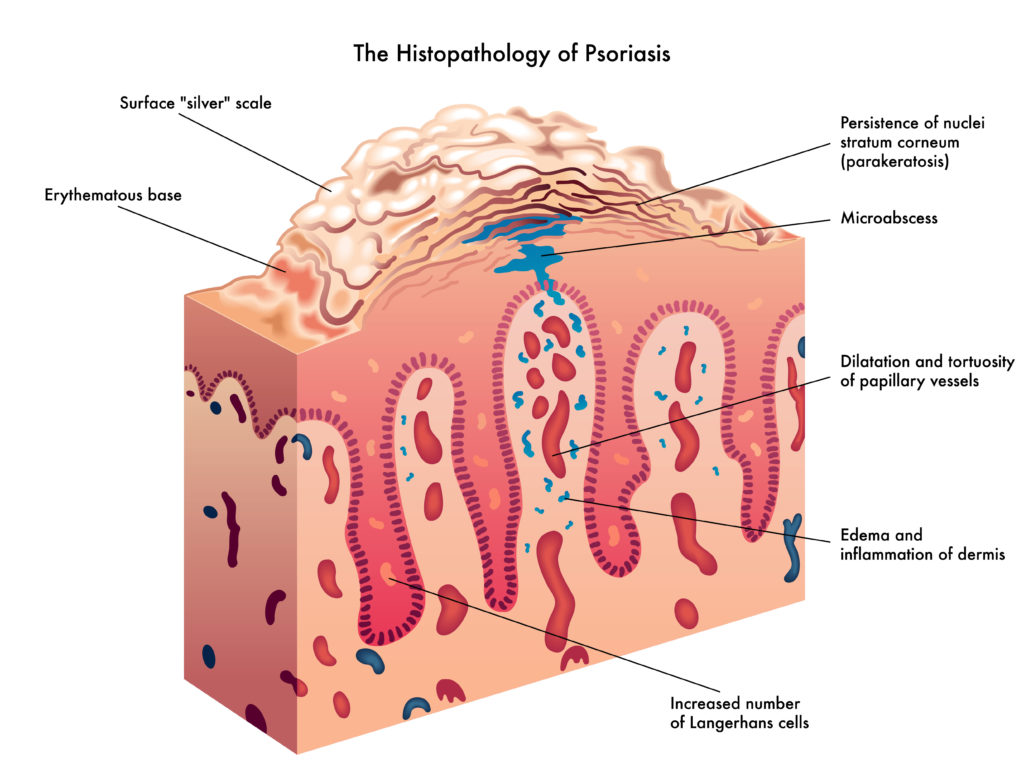
- They grow about five to ten times faster than normal skin cells.
- Due to the quick overproduction of cells, your body can’t keep up because older skin cells don’t have time to fall off. The new skin cells are produced so quickly that they reach the surface of the skin before they’re mature so the old ones are pushed and piled up to the skin’s surface, resulting in thick, flaky, itchy, and burning patches.
- With Psoriasis you have a higher chance of having
-
- Psoriatic Arthritis, (which causes joint pain, stiffness, and swelling, and joint deformity),
- Type 2 diabetes
- Heart Disease (irregular heartbeat)
- Depression
- eye problems (uveitis, blepharitis)
- high cholesterol
- metabolic syndrome
-
- The definite cause of psoriasis is still unknown but the inflammation deep inside the body may trigger the symptoms of psoriasis up to the skin’s surface
- It can affect mental health because of stress, pain, fatigue, and sleeplessness.
COMMON SIGNS AND SYMPTOMS:
- Red patches of skin covered with thick, silvery spots
- Small red or scaling spots
- Dry, cracked skin that sometimes may bleed
- Itching and burning patches
- Thickened, broken nails
- Painful, swollen and stiff joints
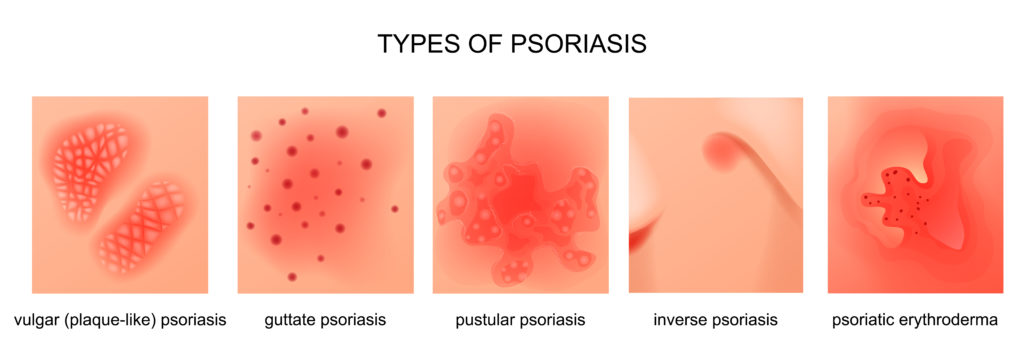
SEVEN (7) TYPES OF PSORIASIS:
1). Plaque Psoriasis
- Also known as Psoriasis Vulgaris, is the most common type.
- Plaque psoriasis can show up as dry, red, raised, and scaly skin patches.
- Plaques may itch or hurt.
- Plaque psoriasis can be mild, moderate, or severe
- Plaque psoriasis often shows up in these areas:
-
-
- Elbows
- Knees
- Scalp
- Knuckles
- Lower back
-
-
2). Pustular Psoriasis
- Pustular psoriasis is uncommon.
- It is characterized by an elevated skin rash that is filled with noninfectious pus (pustules). The skin under and around the pustule is red.
- Make your skin red, painful, and tender
- Common in adults and rare in kids.
- This type of psoriasis may be limited to one area of your body, such as the hands and feet. But when it covers most of the body, (generalized pustular psoriasis), see your doctor right away.
Symptoms include:
-
-
- Fatigue
- Fever
- Chills
- Nausea
- Diarrhea
- Increased heart rate
- Excessive itching
-
Types of Pustular Psoriasis and Symptoms:
Palmoplantar pustulosis (PPP):
-
-
- Small blisters that commonly appear on your palms or soles of your feet.
- Smokers are more prone to getting this type.
-
Acropustulosis:
-
-
- Small and painful lesions
- Forms on fingertips or toes.
-
Generalized or Von Zumbusch:
-
-
- Red, painful, pus-filled blisters that can appear on any part of your body,
- May be very itchy.
- May have fatigue, fever, chills, headache, muscle weakness, joint pain, increased heart rate.
- This is a rare, serious type of pustular psoriasis
-
***Some patients need to be in the hospital if they have this type of psoriasis because it can be life-threatening. It may strain the heart. Rest and hydration are very important.
3). Inverse Psoriasis
- They are lesions or skin rashes that are bright red, shiny, smooth (don’t have scales, no crusting, no pustules, neither dry nor raised)
- This type is also called hidden psoriasis. It usually appears in deep skin folds of the body such as
-
- Armpits
- Groin
- Common under the breast
- Around the genitals and buttocks
-
- More common in people who are overweight because they tend to have deep skin folds
- Gets worse with friction, skin rubbing, and sweating
- It is moist to touch because of sweating and that increases the risk of getting yeast, fungal, and bacterial infection.
Care and Management:
-
-
- Wear loose and made from cotton clothing to let the skin breath
- Baby powder, cornstarch, and baking soda can be applied to the affected area to help absorb moisture
- As prescribed by your doctor, apply diluted topical steroids with anti-yeast or antifungal ointments.
- OTC cooling and anti-itch lotion or mild unscented moisturizer mixed with prescribed topical steroid can be of help to itch and pain
-
4). Guttate Psoriasis
- Small, round, pink-red scaly elevated spots on your skin
- The rashes are not as thick as plaque psoriasis
- The second most common type of psoriasis
- Start from childhood to young adulthood.
- They usually show up on your:
-
-
- Stomach
- Chest
- Face
- Ears
- Arms
- Thighs and legs
- Scalp
-
- Doesn’t appear on your palms, soles of your feet, or on your nails
- You may get it only once and go away without treatment or you could have repeated episodes.
- In some cases, they don’t go away and require medical treatment to control the symptoms.
- It’s usually triggered by an infection
Causes and Triggers:
-
-
- Bacterial Infection – such as streptococcus (strep throat).
- Upper respiratory infections
- Tonsillitis
- Stress
- Cuts on your skin
- Drugs (antimalarials and beta-blockers)
-
5). Erythrodermic Psoriasis
- The least common type of psoriasis
- Most severe type
- It is a serious and dangerous type
- Can be life-threatening
- More common on older people
- Affects men more than women
- Rashes that looks like a sunburn with peeling, covers almost all parts of your body and requires immediate medical attention
- It causes body fluid and protein loss because of peeling off of large areas of skin, similar to a sunburn (may require intravenous fluids because of dehydration).
Symptoms:
-
-
- Severe pain, intense burning, and itching,
- Red and warm to touch the skin
- Looks like a sunburn with peeling
- Increased heart rate
- Fluctuating body temperature
-
Complications:
-
-
- Infection due to peeling off skin that makes the body susceptible to invasion of bacteria or viruses. (may need antibiotics)
- Pneumonia
- Congestive heart failure
- Fluid retention – swelling on ankles
-
Causes and Triggers:
-
-
- Abrupt discontinuation of taking your systemic medications for psoriasis
- Stress
- Severe sunburn
- Alcohol consumption
- Smoking
- Allergic reaction to drugs
- Excessive use of corticosteroids
-
Medical Treatment and Management:
-
-
- Topical steroids
- Moisturizers and lotions with oatmeal or salicylic acid
- Light therapy or phototherapy (UV light therapy)
- Systemic medications – the most effective treatment to control the symptoms.
- A combination of 2 or more of these treatments is usually needed for better control of inflammation.
-
6). Nail Psoriasis
- Most often, people with plaque psoriasis also develop nail psoriasis
- Nail psoriasis looks like a fungal infection, such as onychomycosis.
Symptoms of Nail Psoriasis
-
-
- Thick, brittle and irregularly shaped fingernails caused by a fungal infection
- Ridges in the nails
- Nail is peeling away from the nail bed due to the formation of chalky materials underneath the nails
- Pits or tiny dents like a pinprick hole on the nails
- Discoloration of nails – white, yellow or brown
-
Care and Management for Nail Psoriasis
-
-
- Keep toenails and fingernails trimmed short and clean to prevent fungus and bacteria. Used nail file to smoothen edges and surfaces.
- Soak toenails and fingernails with an antibacterial solution with an added small amount of soap to soften the nail surfaces and make it easier to get rid of the dirt
- Avoid sharp instruments in cleaning your nails to prevent injury, that may cause an infection
- Applying fragrance-free and thick creams, lotions and moisturizers helps keep the nails soft
- Wear comfortable shoes. Recommended round-toed shoes to give enough room to your toes.
- Don’t wear artificial nails, to avoid irritation and invasion of fungus and bacteria
- Wear latex-free gloves to protect your nails when working with bleaches and other cleaning agents.
-
Treatments for nail psoriasis
-
-
- Topical-Cream, ointments or lotions with steroid or salicylic acid applied underneath and around the nails
- Systemic Drugs – Oral drugs- that includes antifungal drugs /antibacterial to treat fungal and bacterial infections
- Biologics- drugs given through injections
- Phototherapy
- Extracting the affected nail
-
*** Nails grow back slowly, that is why the nails take time to heal.
7). PSORIATIC ARTHRITIS
- Psoriatic arthritis is a type of arthritis that targets people who have psoriasis- an autoimmune skin disorder with symptoms of dry, red, raised scaly skin patches.
- It is a disorder where you have both psoriasis and arthritis.
- People have psoriasis first for several years before getting psoriatic arthritis
- The majority of people with psoriatic arthritis also have nail psoriasis.
- Affected joints if left untreated may be disabling or may cause permanent deformity
- Symptoms may be mild to severe
- Risk of having a cardiovascular disease is higher
- People with psoriatic arthritis may also develop:
-
- pinkeye (conjunctivitis) or uveitis
-
Symptoms:
-
-
- Swollen, stiff, and painful joints may be disabling or may cause permanent deformity if not treated.
- Painful and stiff joints are worse in the morning
- Swelling of the fingers and toes
- There is limited mobility due to inflamed or swollen, painful and stiff joints
- Inflamed joints are warm to touch.
- Foot pain
-
- back of your heel (Achilles tendinitis) or
- the sole of your foot (plantar fasciitis).
-
- Low back pain
- Often it could lead to spondylitis
-
Medications for Psoriatic Arthritis
-
-
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
-
- relieve pain and
- reduce inflammation.
-
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
-
-
-
-
-
- Over-the-counter NSAIDs include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Higher doses of NSAIDs require a prescription.
- Side effects may include gastric upset/ irritation, and liver and kidney damage.
-
-
-
-
-
- Disease-modifying antirheumatic drugs (DMARDs).
-
- Helps in slowing down the progress of psoriatic arthritis
-
- Disease-modifying antirheumatic drugs (DMARDs).
-
-
-
- Biologic Drugs
- Steroid injections.
-
-
-
-
-
- reduces inflammation quickly and is oftentimes injected into the affected joint.
-
-
-
CAUSES OF PSORIASIS
I. IMMUNE SYSTEM
A person with healthy skin will produce new skin cells and shed old ones in a process that normally takes about a month. A person with psoriasis produces skin cells at an accelerated rate.
This is because of that person’s immune system being overactive, causing excess inflammation. The inflammation forces the body to produce new skin cells much faster than normal, up to seven times faster than normal. This results in new skin cells being produced in a 4-to-5-day cycle. The body cannot shed older skin cells at this rate, resulting in the new skin cells rapidly piling up as they are pushed to the surface.
These piled up skin cells become the scales and plaques seen on the skin. This build-up can be silvery, red, itchy, flaky, or raised and inflamed. That is how inflammation deep in the body can contribute to the symptoms that show up on the skin’s surface
II. GENETICS
- The risk of developing psoriasis is higher if you have an immediate family member with psoriasis
- Having two parents with the disease greatly increases the risk of getting the disease
III. TRIGGERS
- Stress –
-
- Stress can impact your immune system, a high level of stress may increase your risk of psoriasis
- stress can cause symptoms to appear or make them worse
-
- Smoking –
-
- Smoking tobacco increases your risk of psoriasis and increases the severity of the disease as well;
- smoking makes it harder to treat symptoms.
-
- Alcohol-
-
- heavy drinkers are shown to have a higher risk of psoriasis.
- alcohol can lessen the effectivity of treatments.
-
- Viral and bacterial infections –
-
- People with viral and bacterial infections like HVIare more likely to develop.
- Strep can increase your risk of psoriasis.
-
- Obesity – Overweight increases your risk of psoriasis.
- Vitamin D deficiency
COMPLICATIONS OF PSORIASIS
People with psoriasis, have a higher risk of developing other diseases. These include:
-
- Type 2 diabetes.
- High blood pressure.
- Cardiovascular Disease
- Eye disorders
- conjunctivitis,
- blepharitis
- uveitis
- Obesity
MEDICAL TREATMENTS FOR PSORIASIS
Notes to remember:
- There is currently no permanent cure for psoriasis
- Treatments are available to alleviate the inflammation, scaling, pain, itching, and other psoriasis symptoms.
- Medications effective for other people may not be effective for you.
- A person with psoriasis may have to experiment with multiple treatments to find the one that is most effective to them
1) Topical Treatments
- for a mild-to-moderate form of psoriasis
- slows the rapid growth of skin cells
- applied directly to the affected area
- In the form of oils, gels, ointments, or creams,
- usually the first-line option of treatment for psoriasis.
- helps decrease inflammation and building up plaque.
2) Light Therapy or Phototherapy
- UV phototherapy, or light treatment.
- Uses special lamps that produce UV rays onto plaques/scales
- Helps slow the fast growth of skin cells.
3) Oral Systemics
- treatment choice for moderate-to-severe psoriasis.
- comes in either pill or liquid form acts on the immune system to reduce inflammation.
4) Biologic Treatments
- For moderate-to-severe psoriasis.
- in the form of an injection or infusion
- helping to reduce inflammation.
HOME CARE AND MANAGEMENT
- Hydration- drink plenty of fluids
- Good skincare and good skin hygiene
- Daily Bath. Bathing daily helps get rid of some scales and helps soothe the skin. Avoid hot showers as it reduces the moisture and oil of the skin. Use room temperature or lukewarm water with color free and fragrance -free soaps that have 100% olive oil and argan oil. Soak about 10 minutes then gently pat dry skin and moisturize right away;
- Moisturize your skin frequently (as soon as you get out from the shower to lock in moisture) with fragrance-free moisturizing cream with salicylic acid intended for psoriasis- there are a lot of different brands to choose from the pharmacy – with a prescription or OTC lotions, creams and oils like CeraVe psoriasis moisturizing cream, Cetaphil Pro Soothing moisturizer, Aveeno lotion with oatmeal, Vaseline, Lubriderm Intense Lotion, Eucerin Calming Lotion to mention a few.
-
-
- Don’t use light lotion because it contains a small number of emollients not sufficient to moisturize psoriasis lesions/plaques
- For the body: Wash your body with mild, unscented but ultra-hydrating body cleansers like Aveeno Moisturizing body wash with oatmeal, 100% pure olive oil body wash, Cetaphil calming body wash, CeraVe Psoriasis cleanser with 2% salicylic acid, Soap bars that are fragrance-free and color-free with 100% olive oil and argan oil to name a few.
- For the face: there are plenty of facial washes intended for psoriasis. Use a mild hydrating facial cleanser that will not interrupt the skin barrier like CeraVe hydrating facial wash, Cetaphil facial wash, Eucerin, Lubriderm, Aveeno on top of the lists.
- Don’t use an exfoliant
-
-
- For scalp care: Argan oil has antifungal, antioxidant, and anti-inflammatory properties. Apply to your scalp where plaques are visible and leave it for a few minutes to soften and moisturize the patch before shampooing.
-
-
- Olive oil (dab it to your scalp where plaques are present – soak the scalp before shampooing.
- Tea tree oil (dilute it with your shampoo).
- You can use a dandruff shampoo.
-
-
- Apply a cool compress on an itchy spot or areas that hurt
- Take oatmeal baths to smoothen or soften dry itchy patches
- Get some sunshine between 7 am to 9 am
- (sunlight is beneficial to psoriasis symptoms)
- Avoid sunshine from 10 am to 3 pm
- Avoid cold weather and air conditioning as it will cause dry skin
- Avoid hot showers as they reduce the moisture and oil of the skin
- Diet modification
-
-
- Lean meats in moderation
- Low-sodium foods
- Low-fat dairy
- Low fats
- More fruits
- More on grains esp. whole wheat
- Eat more dark leafy vegetables
- Increase consumption of omega-rich foods – (fish)
-
-
- Relieving stress
-
-
- music therapy- listen to calm music
- meditation
-
-
- Avoiding habits that can cause flare-ups and worsen psoriasis such as
-
-
- smoking (cut down or quit)
- alcohol consumption (cut down or quit)
-
-
- Be careful with your skin. Never pick or scratch patches or scales, as you may make it bleed and make your psoriasis worse. Be extra careful when trimming your nails, make sure not to cut yourself, because it can lead to infection and will worsen your symptoms.
- Maintain a healthy weight.
-
-
- A healthy weight means less strain on your joints
-
-
- Regular Exercise.
-
-
- Exercise can help keep your joints flexible
- Keeps your muscles strong.
- biking, swimming, and walking are examples of non-stressful exercise
- Divide exercise or work activities into short segments to avoid getting exhausted or becoming too tired.
-
-
- Smoking cessation.
-
-
- Smoking can lead to a higher risk of developing psoriasis with more severe symptoms
-
-
- Quit or limit alcohol consumption.
-
-
- Alcohol increases your risk of psoriasis,
- Reduces the effectiveness of your treatment
- It can worsen the side effects of some medications.
-
-
RECOMMENDED DIET FOR PSORIASIS
1). Eat more:
-
- Dark green leafy vegetables
- Fish
- Whole Grains
- Low-Fat Dairy Products
- Olive Oil
- Fruits
- Beans
- Nuts
2). AVOID FOOD THAT CAN CONTRIBUTE TO INFLAMMATION:
-
- Fatty Red Meat
- Sugar and Sweet
- Fried Food:
- Refined Grains:
- Egg Yolks:
- Processed foods
- High Fat Dairy Food:
VITAMINS FOR PSORIASIS
-
- Vitamins A
- Vitamin B
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Fish Oil- Omega 3
CBD and PSORIASIS
-
- Is Cannabis (marijuana) an effective treatment for psoriasis?
- Some research indicates that cannabis decreases the severity of inflammation associated with autoimmune disorders like psoriasis.
- But cannabis experts say that studies are encouraging, but they’re nowhere near conclusive.
***Many types of skin disorders can be prevented or controlled with a healthy lifestyle.